Subtitles & vocabulary
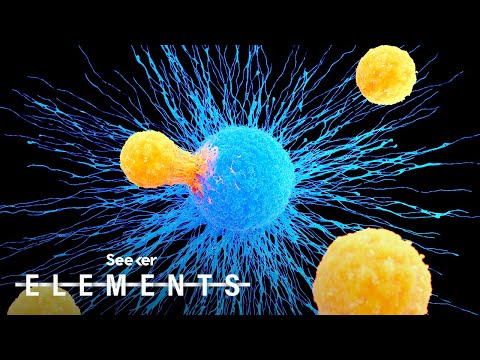
This Cell Might Hold the Answer to a Universal Cure for Cancer
00
Summer posted on 2020/08/28Save
Video vocabulary
specific
US /spɪˈsɪfɪk/
・
UK /spəˈsɪfɪk/
- Adjective
- Precise; particular; just about that thing
- Concerning one particular thing or kind of thing
A2
More potential
US /pəˈtɛnʃəl/
・
UK /pəˈtenʃl/
- Adjective
- Capable of happening or becoming reality
- Having or showing the capacity to develop into something in the future.
- Uncountable Noun
- someone's or something's ability to develop, achieve, or succeed
A2TOEIC
More immune
US /ɪˈmjoon/
・
UK /ɪˈmju:n/
- Adjective
- Having a special protection from, e.g. the law
- Protected against a particular disease or condition because of antibodies or vaccination.
B1
More recognize
US /ˈrek.əɡ.naɪz/
・
UK /ˈrek.əɡ.naɪz/
- Transitive Verb
- To accept the truth or reality of something
- To consider something as important or special
A2TOEIC
More Use Energy
Unlock Vocabulary
Unlock pronunciation, explanations, and filters
