Subtitles & vocabulary
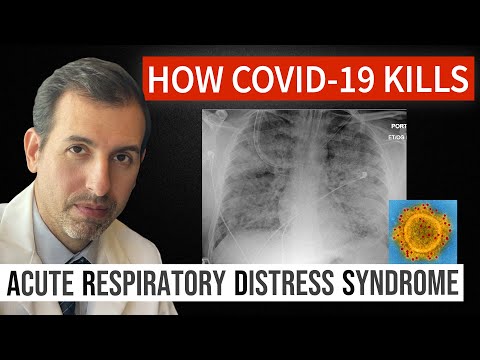
How Coronavirus Kills: Acute Respiratory Distress Syndrome (ARDS) & Treatment
00
Mia Chang posted on 2020/02/25Save
Video vocabulary
entire
US /ɛnˈtaɪr/
・
UK /ɪn'taɪə(r)/
- Adjective
- Complete or full; with no part left out; whole
- Undivided; not shared or distributed.
A2TOEIC
More respiratory
US /ˈrɛspərəˌtɔri, -ˌtori, rɪˈspaɪrə-/
・
UK /ˈrespərəˌtɔ:ri:, -ˌtəʊri:, rɪˈspaɪərə-/
- Adjective
- (Medical) concerning breathing
- Having the function of respiration.
- Noun
- The branch of medicine concerned with the organs of respiration.
- The system of organs involved in breathing.
C1
More position
US /pəˈzɪʃən/
・
UK /pəˈzɪʃn/
- Noun (Countable/Uncountable)
- Person's opinion or attitude about something
- Specific location where someone or something is
- Transitive Verb
- To put in a particular location or direction
- To put or arrange (someone or something) in a particular place or way.
A1TOEIC
More barrier
US /ˈbæriɚ/
・
UK /'bærɪə(r)/
- Noun
- Difficult situation preventing something happening
- Structure or object that stops free movement
B1TOEIC
More Use Energy
Unlock Vocabulary
Unlock pronunciation, explanations, and filters
